Healthcare organizations depend on effective medical data archiving to deliver safe and efficient patient care daily. Every consultation and treatment creates digital records that must remain accessible long-term.
This data lives across electronic health records, imaging systems, billing platforms and legacy applications. Over time, historical data begins to overwhelm active healthcare systems.
Databases grow larger while system responsiveness slowly declines.
Due to this, healthcare leaders face a complex challenge at this stage. Additionally, they cannot remove data due to regulatory and legal obligations. Maintaining legacy platforms only for historical access increases operational risk. Security controls weaken as vendor support ends and patches stop arriving.
Archiving plays a critical role in long-term healthcare data strategy. It supports regulatory compliance while reducing infrastructure strain. It also prepares data foundations for analytics and future innovation.
If your systems feel harder to maintain each year, archiving deserves attention. Go through this blog and get to know more about all of it!
What is healthcare data archiving?
Healthcare data archiving is a structured way to store inactive data. It involves archiving medical records by moving older patient information from active systems into secure, long-term storage. The goal is simple: keep data safe, keep it accessible, and reduce the load on clinical systems.
Healthcare platforms create huge data streams. EHRs grow each hour. Imaging systems expand each minute. Legacy apps continue to hold sensitive patient history. Not all this data needs daily access. But none of it can vanish. This is where archiving works best.
An archive does not delete data. It preserves it. It stores it in formats built for long retention. It supports fast search when clinicians need past records. It reduces cost because archived data uses cheaper storage tiers. It improves performance because active systems hold only active data.
A healthcare archive must follow strict rules. It must protect PHI. It must prevent tampering. It must log every access. It must support clinical audits. It must comply with retention laws across regions and specialties.
Think of it as a library. A place where everything lives in order. A place where you find old records without stress. A place that supports care, even when the original system is gone.
Most healthcare teams reach this point after a major shift. A new EHR. A cloud migration. A system sunset. A compliance review. They realize they need a safe, scalable way to hold data they no longer use daily but still must keep.
That is the core idea behind healthcare data archiving. It is not storage. It is not a backup. It is a strategy for long-term access, trust and operational stability.
How is healthcare data archiving different from backup or retention?
Many teams mix these terms. It leads to confusion. It creates risk. Each method serves a different purpose. Each protects data differently.
A backup is a short-term safety copy. It protects data from sudden loss. It helps during system crashes, outages or accidental deletions. Backups change often. They store live snapshots. They are not built for long-term access.
Retention is a legal rule. It defines how long healthcare data must stay available. It varies by region. It changes by specialty. It controls what must stay, what can go, and when systems must release records. Retention is about compliance, not storage design.
Archiving sits in the middle. It meets retention rules. It stores old data in stable formats. It reduces load on primary systems. It supports fast retrieval when someone needs older records. It keeps PHI safe, organized, and audit-ready.
Here is the simplest way to see it:
- Backups restore systems.
- Retention sets rules.
- Archiving preserves long-term data.
A backup cannot replace an archive. It cannot handle years of inactive data. It cannot support clinical audits or legal reviews. It cannot index data for structured search.
Archiving solves that gap. It moves inactive data into secure storage. It maintains access without slowing active systems. It supports compliance through structured workflows.
Think of it this way. Backups save your day. Archiving protects your future. Retention laws guide both.
Most healthcare teams discover this difference when their EHR slows down. Or when storage costs rise. Or when auditors request records from systems that no longer exist. The right archiving strategy prevents these stress points.
Why should healthcare organizations archive data in 2026?
Healthcare organizations must prioritize data archiving in 2026 as data volumes explode at 36% CAGR through 2025, with healthcare generating over 2,300 exabytes annually and hospitals producing 137 terabytes daily—far outpacing IT budgets and headcount.
Nearly universal EHR adoption (96% of US hospitals) drives this growth from 31 billion USD in 2024 to 46 billion USD by 2032, overwhelming active systems with new formats, compliance rules like HIPAA, and imaging records that can’t be deleted.
Legacy systems amplify the crisis: 83% of IT teams report daily operational disruptions, consuming up to 75% of budgets on maintenance while exposing 70% of breaches and costing millions per incident. Archiving addresses this head-on by offloading inactive data to low-cost tiers, slashing storage and infrastructure expenses by 30-50%, boosting EHR and imaging query speeds, and enabling legacy shutdowns without losing auditable history.
The payoff is swift providers see ROI in 12-24 months through lighter workflows, easier audits and readiness for analytics markets surging to 146 billion USD by 2032. In 2026, delaying means higher risks and costs; archiving transforms data from burden to asset, restoring performance and compliance confidence.
What kinds of healthcare data need archiving?
Healthcare organizations handle diverse data types across clinical and operational environments.
Most of this data becomes inactive over time but remains subject to retention requirements.
Identifying the right data for archiving reduces risk and improves system performance.
Healthcare data commonly requiring archiving includes:
- Electronic Health Records (EHR data)
Older patient encounters lose daily relevance but retain long-term clinical importance. Regulations require continued access for audits and continuity of care needs. - Medical imaging data
Imaging files consume significant storage after treatment completion. Archiving preserves diagnostic history without slowing active imaging platforms. - Revenue cycle and billing data
Billing records support audits and dispute resolution activities. Keeping them in active systems increases cost without operational benefit. - Laboratory data
Historical lab results support future clinical reviews and research initiatives. Archiving maintains access without overwhelming laboratory information systems. - Administrative and operational data
Staff records and operational documents still carry retention obligations. Archiving secures this information while reducing exposure in active environments. - Legacy application data
Older systems often fail modern security and performance expectations. Archiving enables safe system retirement without losing historical access.
A structured data classification approach simplifies archiving decisions. Teams identify inactive datasets using access patterns and regulatory requirements. This prevents unnecessary retention inside high-cost production systems.
Governance frameworks further strengthen archiving effectiveness. Clear policies align compliance, IT and clinical stakeholders. They also enable faster responses during audits and data requests.
Why should healthcare organizations archive data in 2026?
Healthcare organizations must prioritize data archiving in 2026 as data volumes explode at 36% CAGR through 2025, with healthcare generating over 2,300 exabytes annually and hospitals producing 137 terabytes daily far outpacing IT budgets and headcount.
Nearly universal EHR adoption (96% of US hospitals) drives this growth from 31 billion USD in 2024 to 46 billion USD by 2032, overwhelming active systems with new formats, compliance rules like HIPAA, and imaging records that can’t be deleted.
Legacy systems amplify the crisis: 83% of IT teams report daily operational disruptions, consuming up to 75% of budgets on maintenance while exposing 70% of breaches and costing millions per incident.
Archiving addresses this head-on by offloading inactive data to low-cost tiers, slashing storage and infrastructure expenses by 30-50%, boosting EHR and imaging query speeds and enabling legacy shutdowns without losing auditable history.
The payoff is swift—providers see ROI in 12-24 months through lighter workflows, easier audits and readiness for analytics markets surging to 146 billion USD by 2032. In 2026, delaying means higher risks and costs; archiving transforms data from burden to asset, restoring performance and compliance confidence.
How does the healthcare data archiving process work?
Health data archiving follows a structured and repeatable process. Each step ensures data security, compliance and long term accessibility.
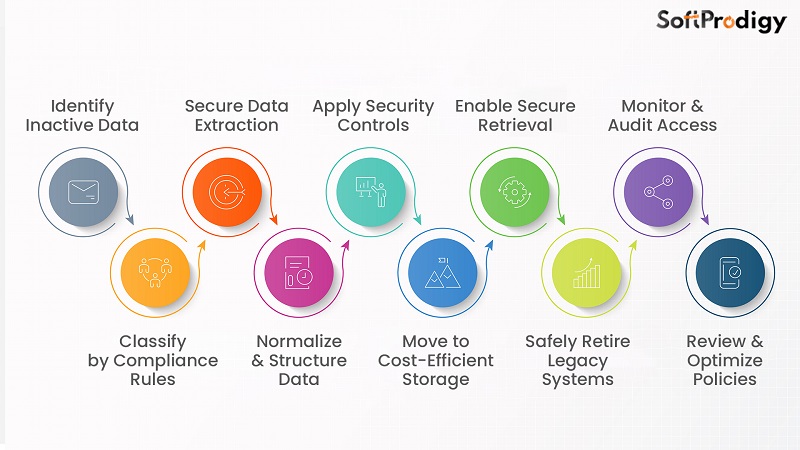
Step 1: Identify inactive healthcare data
Most healthcare systems contain large volumes of rarely accessed historical records. Industry studies show nearly 70 % of healthcare data becomes inactive after two years. Usage patterns help teams identify records no longer required for daily operations.
Step 2: Classify data based on regulatory requirements
Different healthcare data types follow different retention rules globally. Patient medical records often require retention ranging between 7 to 10 years. Classification ensures data meets legal and clinical access obligations.
Step 3: Extract data from source systems
Inactive data is securely extracted from EHRs and legacy platforms. This process avoids disruption to live clinical workflows. Extraction typically occurs during controlled maintenance windows.
Step 4: Normalize and structure archived data
Archived data is converted into standardized and readable formats. Metadata is applied to support search and audit requirements. Structured data improves retrieval speed during clinical or legal requests.
Steps like data normalization and controlled retrieval are essential parts of clinical data archiving, ensuring that historical clinical information remains usable and accessible.
Step 5: Apply security and compliance controls
Archived healthcare data requires the same protection as active data. Encryption is applied both during transfer and storage. Access controls ensure only authorized users can retrieve sensitive information. According to industry benchmarks, encrypted archives reduce breach exposure by over 40%.
Step 6: Store data in cost-efficient environments
Archived data moves to storage tiers designed for long-term retention. These environments cost significantly less than high-performance production systems. Organizations report storage cost reductions between 30 and 50 percent after archiving.
Step 7: Enable controlled data retrieval
Archived data remains searchable through secure interfaces. Clinicians retrieve records during follow-up care or historical reviews. Compliance teams access data quickly during audits or legal inquiries.
Step 8: Decommission legacy systems safely
Once data is archived, outdated systems can be retired. This reduces maintenance costs and security risks. Healthcare organizations save millions annually by eliminating unsupported platforms.
Step 9: Monitor and audit archived data access
Continuous monitoring tracks every access request. Audit logs support regulatory reporting and internal governance needs. This visibility strengthens trust across compliance and leadership teams.
Step 10: Review and optimize archiving policies regularly
Healthcare data volumes continue growing each year. Archiving policies require regular updates to remain effective. Ongoing reviews ensure alignment with evolving regulations and organizational needs.
If this process feels complex, structured support makes a difference. SoftProdigy helps healthcare organizations implement compliant archiving workflows. A guided approach reduces risk while accelerating modernization efforts.
How long must healthcare data be retained or archived?
Healthcare data retention timelines vary based on regulations, data type and jurisdiction. Organizations must follow legally defined retention periods to remain compliant. Failure to meet retention rules can trigger audit and legal exposure.
Retention timelines typically depend on the following factors:

1. General medical records
Most healthcare regulations require adult patient records to be retained for extended periods. Retention commonly ranges between 7 to 10 years after the last patient encounter. Archived records must remain accessible throughout the entire retention duration.
2. Pediatric medical records
Pediatric records often require longer retention due to patient age considerations. Many regions mandate retention until the patient reaches adulthood plus additional years. This can extend retention timelines to 18 to 25 years in some jurisdictions.
3. Diagnostic imaging records
Imaging data retention depends on clinical relevance and local regulations. Common retention periods range between 5 to 7 years after imaging completion. Some specialties require longer retention based on patient risk profiles.
4. Billing and financial records
Healthcare financial records support audits and dispute resolution activities. Retention periods typically range between 6 to 10 years globally. Archived billing data must remain retrievable for regulatory and payer reviews.
5. Clinical trial and research data
Research data follows stricter and longer retention rules. Regulations often require retention for 15 years or more after study completion. Archived access supports regulatory inspections and future scientific validation.
6. Employee and operational healthcare records
Human resources and operational data also carry retention obligations. Retention timelines vary based on labor laws and healthcare regulations. Archived access supports investigations and compliance verification processes.
What storage and architecture options exist for healthcare data archiving?
Healthcare data archiving requires storage architectures built for security and long-term access. The right architecture balances cost, performance, and regulatory compliance.
Organizations choose models based on data volume, access frequency, and infrastructure maturity.
Common healthcare data archiving architecture options include:
1. On-premises archiving architecture
On-premises archives store data within an organization’s own data centers. This model provides direct control over infrastructure and data residency requirements. It suits organizations with strict internal governance or limited cloud adoption.
2. Cloud-based archiving architecture
Cloud archives support faster deployment and reduced infrastructure management effort. They also integrate well with modernization and analytics initiatives. Regulatory compliance depends on proper configuration and vendor alignment.
3. Hybrid archiving architecture
Hybrid architectures offer flexibility during EHR migrations and system transitions. They reduce risk while enabling phased cloud adoption. Governance policies ensure consistent access and security across environments.
4. Object storage for healthcare archives
Object storage is widely used for large healthcare archives. It supports massive scalability and metadata-driven search capabilities. Imaging and document-based records benefit significantly from this structure.
5. Cold storage and tiered storage strategies
Cold storage supports data accessed infrequently over long retention periods. Tiered storage moves data automatically based on access patterns. This approach reduces cost while preserving retrieval capability.
Wrapping Up,
Healthcare data continues growing while regulations demand stronger control and long-term accessibility. Organizations can no longer depend on aging systems to manage this expanding responsibility. Health data archiving brings structure to complex environments by separating inactive records from active systems. This separation improves performance while maintaining secure and compliant access to historical information.
A thoughtful archiving strategy reduces infrastructure cost and operational strain. It strengthens audit readiness and supports regulatory requirements across regions. Archiving also enables modernization efforts such as EHR upgrades and cloud adoption by removing legacy data barriers. Teams regain control over the data lifecycle instead of reacting to constant system pressure.
Organizations that prioritize archiving position themselves for stability and growth. They reduce future risk while building scalable and governed data foundations. Healthcare data archiving is no longer optional in modern IT strategies. SoftProdigy helps healthcare organizations implement compliant archiving solutions that support performance, security, and long-term confidence.













